How might we empower US residents in primary self-care?
︎Client: GoInvo
︎Category: Service Design
︎Type: Professional/White Paper
︎Time: 5 weeks
︎Skills: Research, Design-Thinking Workshop, Digital/Physical Experience
︎Category: Service Design
︎Type: Professional/White Paper
︎Time: 5 weeks
︎Skills: Research, Design-Thinking Workshop, Digital/Physical Experience
︎
Why?
For US Residents:
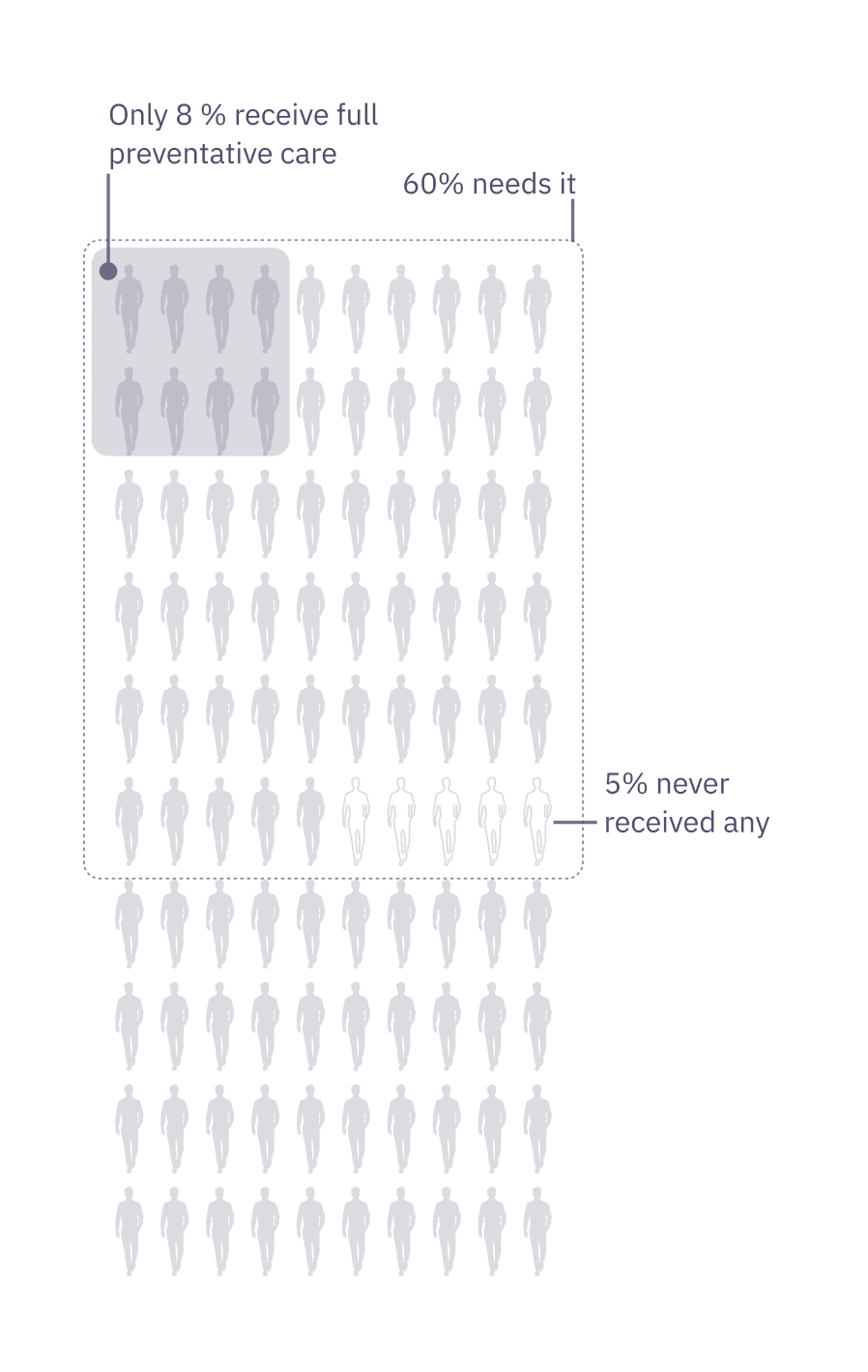
Only 8% of Americans age 35+ have received all of the high-priority clinical preventative services.
16M reported to have received none in 2015.
60% of US residents have at least one chronic disease in 2014.
Lack of preventative care use has been a prolonged issue in the US, and little has changed even with the increased coverage of insured individuals through the Affordable Care Act. Some reasons identified in a 2018 survey for missing care are low levels of trust in physicians, work/family obligations, and long wait times.
We must give US residents the tools to conduct regular primary self-care, to monitor and prevent worsening symptoms of chronic illnesses.
Only 8% of Americans age 35+ have received all of the high-priority clinical preventative services.
16M reported to have received none in 2015.
60% of US residents have at least one chronic disease in 2014.
Lack of preventative care use has been a prolonged issue in the US, and little has changed even with the increased coverage of insured individuals through the Affordable Care Act. Some reasons identified in a 2018 survey for missing care are low levels of trust in physicians, work/family obligations, and long wait times.
We must give US residents the tools to conduct regular primary self-care, to monitor and prevent worsening symptoms of chronic illnesses.
For Department of Health and Servies in US and its Cities/Towns:
Preventative primary care should be integrated into the community, instead of being a strictly clinical effort. City, town, and community leaders can get a better grasp of their resident’s health to better distribute resources and collect evidence for policy making. It’s time to“shift delivery into the community, reaching people where they live, work, learn, and play.” (Krist et. al, 2015)
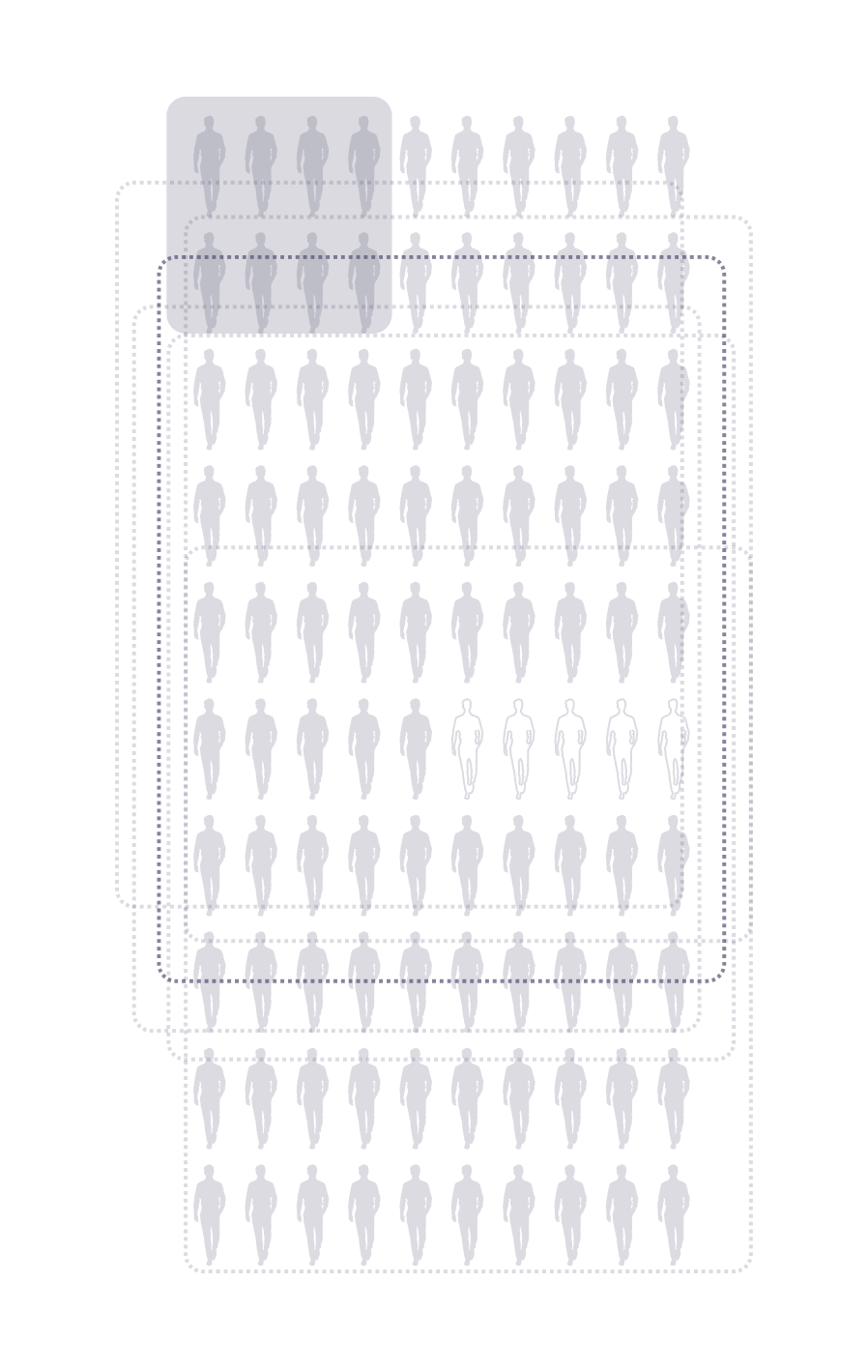
Healthy People 2030, the national objectives has detected little change in increasing preventative care delivery and access. The target is to give evidence-based preventative care to 11.5% of the population by 2030.
Currently it is at 6.5%.
Preventative primary care should be integrated into the community, instead of being a strictly clinical effort. City, town, and community leaders can get a better grasp of their resident’s health to better distribute resources and collect evidence for policy making. It’s time to“shift delivery into the community, reaching people where they live, work, learn, and play.” (Krist et. al, 2015)
Healthy People 2030, the national objectives has detected little change in increasing preventative care delivery and access. The target is to give evidence-based preventative care to 11.5% of the population by 2030.
Currently it is at 6.5%.
—Are we providing resources to those who need it?
︎
How?
From Public Restroom to Public Healthroom
Infrastructure is public health, preventive health, and personal health. Historically, we see this relationship in everything from the reduction of waterborne disease through water sanitation systems to the one-year extension to New York City citizens’ lifespan with added bike lanes.
As healthcare shifts from a focus on treatment to prevention, from quantity to quality, and from mega-medical campuses to local community centers, new infrastructural opportunities continue to arise. One such opportunity is the screening and prevention of chronic illnesses—specifically by evolving the role of public restrooms in health.
Design Process and Logic
The project was developed through an interplay between research and design to make both evidence-based and user-based decisions. This process was aimed at generating idea that is both scalable and human-centric.

Artifacts of Work in the Process
︎Studio Workshop Feedback Session
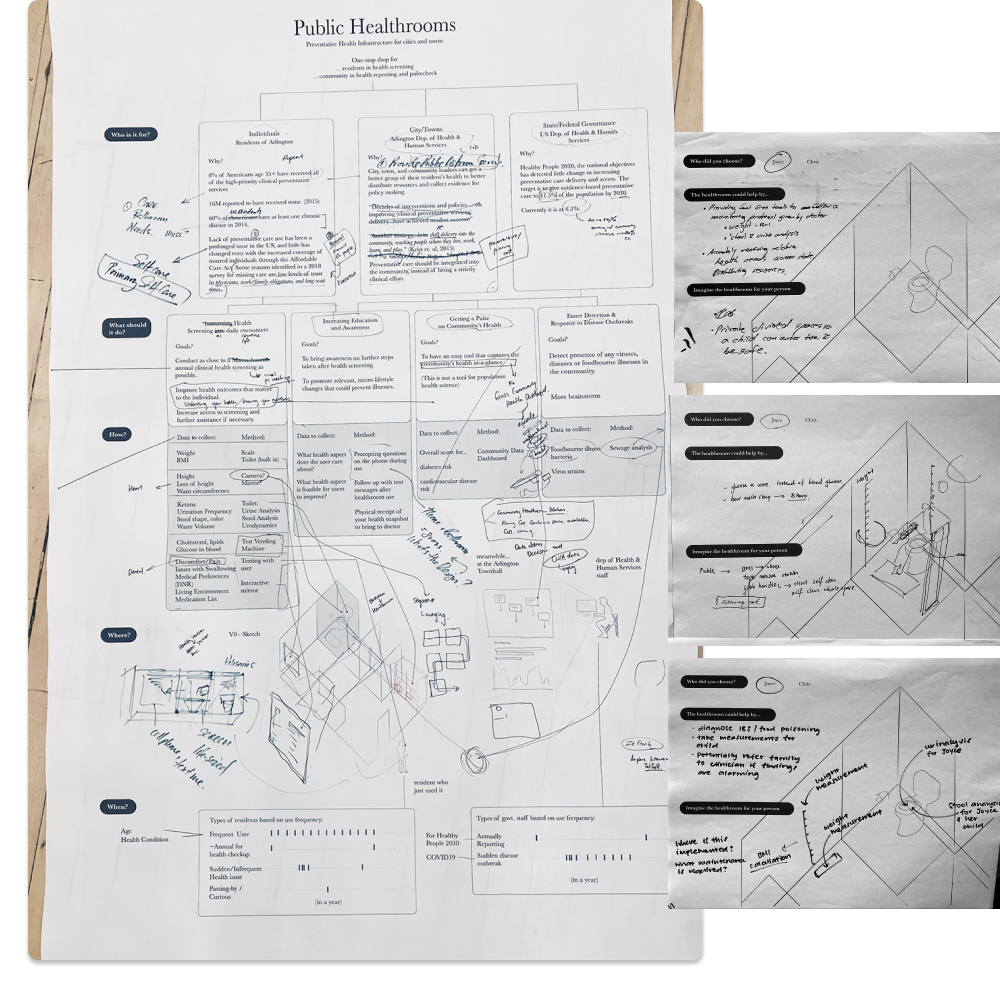
A 30 minute workshop with 10 of the studio members on brainstorming the ideal preventative care episode for two personas and statistics from the Town of Arlington.

︎Public Healthroom’s Four Primary Principles
Residents own their health data. The public healthroom is a means for individuals to access and understand their key physical health indicators, but it protects your privacy and does not sell historical data to third-parties.
All residents should have easy access to preventive care. No one should have to ignore health concerns because of geographic or socioeconomic barriers.
Preventive care must meet residents where they are. The public healthroom bridges the gap between complete self-care and professional hospital care. Based on analysis of a resident’s biometrics across time, the healthroom provides detailed recommendations on seeking the appropriate level of care.
Personal health is relative. The public healthroom helps each individual detect abnormalities in the context of their own history (e.g., sudden weight fluctuation, height loss, vision loss). Uncovering hidden signals can help prevent deterioration of various diseases (e.g., blindness caused by diabetes).
︎Public Healthroom’s Health Model
︎
What?
Hypothesis 1.0 of Implementation

User Experience
System Perspective
The public healthroom is a one-stop shop for US residents to access basic health screening through daily encounters. The room is composed of devices and communication tools that provide screening and risk assessment for common chronic diseases like diabetes and heart attacks.
These devices collect the resident’s biometric data to generate a personal health “receipt” that can indicate health abnormalities, suggest further testing, and provide useful information for follow-up with a primary care physician.
︎
What’s Next?
In the fiscal year 2021-2022, the operation cost of public toilets by San Francisco Public Works was $12.7 million or $113,000 per year per portable toilet that opens 40 hr/week. Using this as a baseline, the public healthroom is susceptible to higher costs to engineer, build and operate beyond the government budget. To actuate the significant value of public healthroom that transitions US healthcare spendings from quantity to quality, a MVP must be developed to analyze potential funding structures (private vs public vs hybrid) and user-testing.
One potential MVP to test the idea is to develop each tool separately:
One potential MVP to test the idea is to develop each tool separately:
- Refurbishing public restrooms or restrooms in community center (YMCA, Student Centers, retail toilets) with urine/stool analysis toilets, following Olive.earth
- Developing a software for screening recommendations based on age and sex, used for retail healthcare (CVS MinuteClinic, Walgreens Health, Walmart Health Center), and integrating with their screening/lab test services
- Aggregating at-home test/finger-prick test vendors into one physical vending machine at retailers and community health centers
By promoting lifestyle changes and increasing preventive care awareness and access, policy makers and care providers are constantly striving to support better health outcomes for all—the Public Healthroom opens up a conversation around seamlessly integrating health into our daily encounters via the built environment. As emergent technologies develop and preventive care needs increase in the next five years, success in implementation and public utilization will rely heavily on design, and on how thoroughly we consider how the experience of engaging with one's health can be seamless and timely without over-complications in technology.